Staging investigations
Imaging of the pancreas
Ultrasound
Pancreatic and biliary ultrasonography is a useful first investigation. It will reveal dilatation of the bile ducts which could represent obstruction to the flow of bile within the head of the pancreas. It can also show a dilated pancreatic duct due to tumour obstructing the flow of pancreatic juice.
Pancreatic cancer occurs in the head of the pancreas in about half the patients and leads to bile duct obstruction. The sensitivity of ultrasonography in pancreatic cancer is as high as 90%. However, ultrasound will often fail to show the entire gland. In particular, tumours that arise in the body and tail of the pancreas may be difficult to see on ultrasound.
CT Scanning
 |
Pancreatic cancer CT Coronal. Black arrow |
Accurate CT scanning or computer tomography requires a multi-slice CT machine. This may well show a focal or diffuse mass in the head of the pancreas. The accuracy of CT in the diagnosis of pancreatic cancer is approximately 90%. CT is good at diagnosing contiguous organ invasion such as duodenum, stomach, or spleen. It will show vascular involvement of the major gut vessels in more than 50% of patients and it will show liver secondaries in nearly half the patients as well.
The findings on CT scanning correlate very well with the findings at surgery and patients deemed inoperable on CT scanning are most likely to be inoperable at exploration as well.
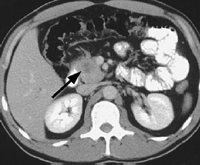 |
Pancreatic tumour on CT scan (arrow). |
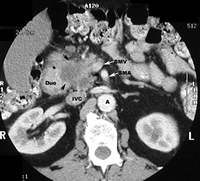 |
Pancreatic tumour on CT scan - More advanced (arrows) and Invading SMV. |
MRI Scanning
 |
Pancreatic cancer - double duct sign showing stricture (narrowing) of bile and pancreatic ducts. |
Although MRI scanning is used to look at the structure of the pancreas it is not a particularly good investigation for this. However, MRCP is extremely effective at looking at the pancreatic duct and biliary tree and images here can be very useful in planning surgery.
ERCP
 |
Pancreatic cancer - showing bile duct stricture. |
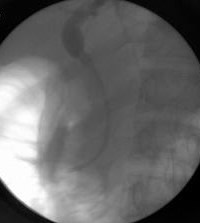 |
Pancreatic cancer stented - Stent in bile ducts. |
ERCP is a special investigation for imaging the bile ducts and the pancreatic duct and it provides complimentary information to that given by other forms of x-ray imaging. In this procedure the patient is sedated and when asleep a duodenoscope is passed through the mouth down the oesophagus or gullet and into the duodenum. An endoscope is positioned opposite the opening of the bile and pancreatic ducts which are then cannulated with a tiny tube and an x-ray performed. This reveals the anatomy of the bile ducts and pancreatic duct. If the patients happens to be jaundiced a plastic tube, or a stent, may be placed through the duodenoscope across the site of blockage to relieve the obstruction. In a patient who has inoperable or incurable disease a self expanding metallic stent may be placed across the bile duct stricture to relieve jaundice. These stents provide better palliation than plastic stents but the disadvantage is that they are not removable.
Although ERCP is a safe procedure, it has a small but finite risk of triggering pancreatitis i.e. inflammation of the pancreas which is a serious complication. In addition, if a procedure is carried out to place a stent or to open the biliary sphincter from within, there is a tiny risk of bleeding or perforation, which may require surgery to repair.
PTC (Percutanous transhepatic cholangiogram)
In patients who are very deeply jaundiced, surgery is not safe and the jaundice must be relieved by stenting. If an endoscopist is unable to stent a narrowing in the bile duct at ERCP then the radiologist will attempt to stent this through a puncture of the liver by the technique of PTC. By puncturing the liver under ultrasound guidance, a wire may be passed into the duodenum through the liver and a stent railroaded across the strictured part of the bile duct. The problems with this procedure include bleeding and leakage of bile from the punctured liver.
 |
Pancreatic cancer related bile duct obstruction - relieved by plastic stent. |
 |
Pancreatic cancer related bile duct obstruction - relieved by metal stent. |
EUS (Endoscopic ultrasound)
 |
Pancreatic cancer seen on EUS. |
By placing an ultrasound probe at the end of an endoscope, which is passed into the duodenum under sedation, the ultrasound probe can be placed very close to the pancreas from within the patient. With this technique excellent images can be obtained of the pancreas and small tumours may be visualised. In addition biopsies may be taken from a tumour to confirm the cell type. Endoscopic ultrasound has improved the staging of pancreatic tumours enormously.
Tumour markers
The CA19-9 tumour marker is useful in diagnosing a large tumour or advanced disease. However it is not of much use in diagnosing early cancers and may on occasion be completing misleading.
Images by courtesy of Dr Anthony Lopez, Consultant Radiologist and CEO of The Imaging Clinic.